11 January 2015
Our
average work day consists of signing out the cases grossed the previous day -
about 20-25 surgical cases (including biopsies), 3-5 cytology cases, and 2-4
peripheral blood smears. There are a couple bone marrow cases and 10-20 pap tests per week. Since
the provided histories are often limited and there is no electronic medical
records, we sometimes go find the patient on the wards and gather information
from the clinicians and chart. Some of the more sophisticated tools available
to us include reliable internet, Olympus microscopes with attached cameras, a
library more complete than that at the Seattle VA Medical Center, Dragon
dictation software and headsets for grossing, a computerized reporting system
(FileMaker), and collegial surgeons who visit us often to discuss their
patients. However, without a doubt, the resource that helps me the most in my
daily tasks, is Ginger Jensen. Ginger diligently and efficiently assists me in
the gross room – triaging cases, labelling blocks, changing blades, cleaning up
messes, pointing out mistakes, confirming patient identifiers, and offering
keen advice about when to consult Rochelle. She is patient and excellent
company.
I am impressed that the hospital
has fairly reliable electricity thanks to a backup generator. Histology labs
are dependent on a significant amount of infrastructure and relatively
complicated equipment. Electricity is required for the slide drying oven,
ventilation fan (to reduce formalin fumes), microscope lights, computers, and
freezing blocks of ice to cool the paraffin blocks prior to microtome
sectioning. Perhaps this is the reason there are so few anatomic pathology labs
in Sub-Saharan Africa. We are not aware of another lab in this region of Kenya,
other than in Nairobi. A critical mass of health care capacity must be reached
before a hospital can support and benefit from an anatomic pathology lab. There
must be surgeons operating consistently enough (and who have the required
operating room infrastructure) to provide enough specimens to justify the
expenditure for technician salaries, equipment purchase and maintenance,
reagents, and space.
The largest barrier to providing
crucial diagnoses to guide surgical treatment is the pathologists themselves.
When Kijabe goes without a volunteer visiting pathologist, they send the
specimens to Aga Khan University Hospital in Nairobi. Many of the specimens
sent there in mid-December have not yet had a diagnosis returned. Like many
medical sub-specialties, training of pathologists in Kenya is complicated by
lack of adequate residency training opportunities. To train the future
generation of Kenyan pathologists, there first has to be enough pathologists to
tend to the diagnostic needs of the country and then enough to have time to
dedicate to teaching. In my opinion, teaching and mentorship is one of the most
sustainable contributions foreign physicians of any specialty can make to a
resource-limited country. Yet, like any action by a well-intentioned
researcher, medical volunteer, missionary, or NGO-organization, even teaching
carries the risk of doing more harm than good. Who can blame a Kenyan physician
who is trained in pathology to seek employment in Dubai, England, or the U.S.
if the opportunity presents itself? The “brain-drain” of medical specialists
occurs because many receive training in Europe where professional and personal connections
develop, which provide routes to leave one’s home country for extended periods
or even permanently.
Here are some cases from the first week:
 |
| #1 Left upper eyelid and nose, biopsy: Dermatofibrosarcoma protuberans (recurrent) invading skeletal muscle and adipose tissue. |
 |
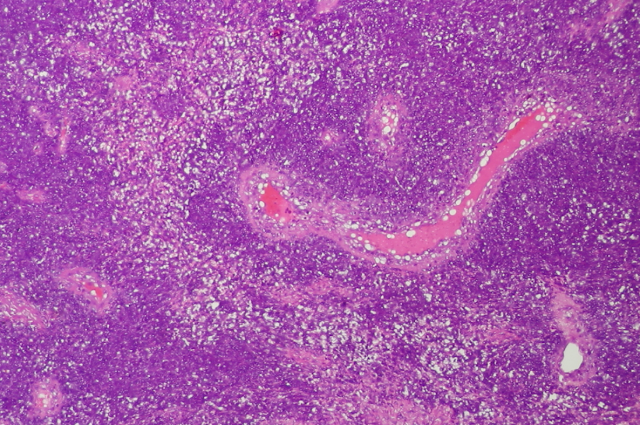
#2
Patient: 3 year old male status post hemimandibulectomy for
jaw mass.
Gross: A tan-white, firm mass (7.0 cm AP x 2.5 cm ML x 3.5 cm SI) has its
epicenter in the mandibular bone. The mandible is fractured posterior to two
molars. The bone is porous and thin.
Diagnosis: Low grade
spindle cell neoplasm, eroding bone and extending to apparent medial and
lateral margins; consistent with a desmoplastic fibroma. Consultation was provided by pediatric pathologists at Seattle Children's Hospital.
| | | |
 |
| #2 High power view of jaw mass |
|
 |
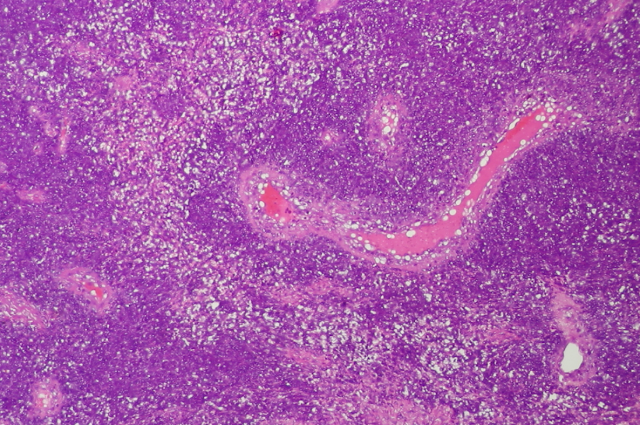
| #3 Patient: 30 year old HIV positive woman. Sharply delineated gluteal and sacral skin ulcer. Lesion spread from initial small vesicle. Photo of the lesion. |
|
 |
| #3 Low power view at interface of normal skin and ulcer. |
 |
#3 High power view
of ulcer.
Diagnosis: Skin,
sacral and gluteal, biopsy: ulcerated skin with neutrophilic inflammation and
epithelial cells with probable viral inclusions, consistent with herpes simplex
virus infection.
|
|
 |
#4 Patient: 36 year old male with slow-growing left elbow
mass.
Diagnosis: Malignant small round blue cell neoplasm. Differential include Ewing sarcoma, neuroectodermal tumor, others. Consultation was provided by UWMC bone and soft tissue pathologists.
|
|
 |
| #5 Peripheral blood smear from pediatric patient with microcytosis (MCV=76 fL) without anemia and numerous target cells. Diagnosis: Thalassemia trait. |
|
Other cases included two chronic myeloid leukemias on peripheral smears, and a multiple other neoplastic pediatric and bone and soft tissue cases.
 |
| My desk on the right and Dr. Garcia's on the left. Excellent library of slightly outdated pathology text books. |
 |
| Slide staining station. |
 |
| Phyllis cutting at the microtome and Peris scooping tissue onto slides from the water bath. |
 |
| Gross bench with computer access to the pathology database and wireless headset for direct dictating. |
 |
| Main door to anatomic path lab. |
 |
| Slide storage corner. |













Thanks for an excellent overview of a representative day in the life of a visiting pathologist. All is well in Montana. The skiing continues to be excellent and winter fishing is reasonably successful.
ReplyDelete